Abstract
Despite many advances, the treatment of acute myeloid leukemia (AML) remains challenging, and few patients are cured by therapies other than allogeneic hematopoietic cell transplant. Treatment with natural killer (NK) cells from allogeneic donors is a promising therapy that can achieve remissions in 30-50% of AML patients. To generate an improved cell-based therapy for AML, our group has produced NK cells from induced pluripotent stem cells (iPSCs). iPSC-derived NK cells effectively kill AML cells, but may benefit from additional modifications or combination with other therapies to durably cure AML. Based on studies that demonstrate that targeting the CD47 pathway on macrophages and NK cells improves anti-tumor activity and is an effective treatment for patients with AML, we investigated the combination of iPSC-derived NK cells with iPSC-derived macrophages with and without CD47 blockade for the treatment of AML.
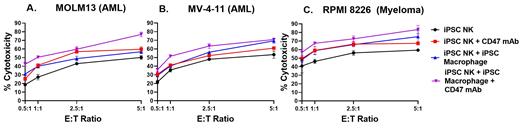
AML clinical trials combining anti-CD47 monoclonal antibodies (mAb) with chemotherapy have demonstrated an anti-tumor effect primarily thought to be mediated though a macrophage immune-checkpoint blockade mechanism. To determine if addition of iPSC-derived macrophages can improve the cytotoxicity of NK cells against AML blasts, we co-cultured iPSC-NK cells and MOLM13 or MV-4-11 AML cells with iPSC-macrophages in a standard cytotoxicity assay. Similar results were found for cytotoxicity tests against both AML cell lines (Figure panels A and B). While macrophages alone did not kill AML blasts, the addition of iPSC-macrophages to iPSC-NK cells significantly improved killing of the AML cells by 50% (p<0.01). Addition of an anti-CD47 mAb (B6H12) further increased killing of these AML cells by the iPSC-NK cell + iPSC-macrophage combination treatment by an additional 23% (p<0.01). Intriguingly, the addition of just the anti-CD47 mAb to the iPSC-NK cells also significantly increased anti-AML activity, although this increased killing was consistently lower than what was seen with addition of iPSC-macrophages combined with anti-CD47 and iPSC-NK cells. Addition of the CD47 mAb to iPSC-macrophages without NK cells did not result in increased anti-AML cytotoxicity. We also demonstrated that blockade of SIRPα (the receptor on NK cells for CD47) significantly increased NK cell killing of AML blasts by 16% (p<0.05). Furthermore, the combination of iPSC-NK cells + iPSC-macrophages + SIRPα mAb led to a 37% increase in cytotoxicity compared to iPSC-NK cells + iPSC-macrophages alone (p<0.01).
To confirm that addition of anti-CD47 or anti-SIRPα antibodies increased NK cell activation via loss of the inhibitory CD47-SIRPα interaction between NK cells and AML blasts and not by another mechanism, we tested the effect of adding both CD47 mAb and anti-SIRPα antibodies. Compared to addition of either anti-CD47 or anti-SIRPα mAb alone, the combination induced no additional increase in anti-AML activity by the NK cells. These results suggest that the CD47-SIRPα interaction between AML and NK cells is an important inhibitory immune-checkpoint on NK cells. To control for the effect of blocking SIRPα on macrophages, we tested the addition of the SIRPα mAb to iPSC-macrophages. This combination did not improve on the lack of cytotoxicity exhibited by macrophages alone. We also evaluated if ADCC mediated by the anti-CD47 mAb binding AML blasts could account for the increase in cytotoxicity and found that blockade of Fc-receptors on NK cells does not diminish the increase in cytotoxicity seen with addition of the mAb, excluding a role for ADCC.
To investigate if these findings with AML could be extended to other hematologic malignancies, we tested the combination of iPSC-NK cells, iPSC-macrophages and CD47 mAb against the RPMI-8226 multiple myeloma cell line (Figure C). Here, we again demonstrate that CD47 blockade combined with iPSC-macrophages leads to increased NK cell-mediated anti-myeloma activity. In vivo studies testing the combination of iPSC-NK cells, iPSC-macrophages and CD47 mAb against human AML and myeloma cells in mouse xenograft-models are ongoing. Together our results indicate that blocking the CD47-SIRPα interaction between NK cells and tumor cells consistently mediates improved anti-tumor activity. Furthermore, iPSC-derived NK cells and macrophages provide an important, standardized, "off-the-shelf" cell therapy approach that can be translated into novel clinical therapies.
Kaufman: Shoreline Biosciences: Consultancy, Current holder of stock options in a privately-held company, Membership on an entity's Board of Directors or advisory committees, Research Funding; Qihan Biotech: Consultancy, Current holder of stock options in a privately-held company; VisiCELL Medical: Consultancy, Current holder of stock options in a privately-held company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal